BACK PAIN
Low back pain (LBP) is the leading cause of disability worldwide. It is a common condition that emerges during adolescence and throughout adulthood. For some, LBP is self limiting and not disabling, but for others, it can be disabling, distressing and negatively disrupts many aspects of life.
The best practice evidenced management of low back pain includes:
-
An initial triage process to screen for serious pathology
-
Screening and profiling a LBP disorder from a broader biopsychosocial perspective so as to identify patients at risk of persistent disabling LBP
-
A patient centered approach LBP care that addresses biopsychosocial influences relevant to their experience and empowering self management
-
Tailored LBP management that encourages patients to be active participants for their recovery
-
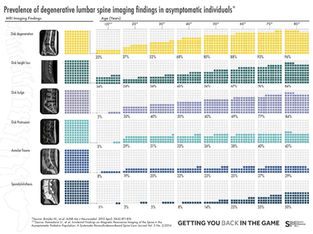
Radiological imaging should only be used when there are clear indications for it such as ruling out for serious, unresolved pathology, red flags of the back.
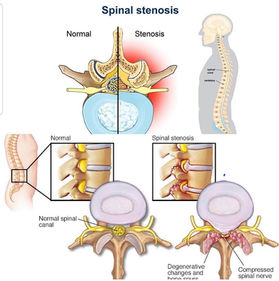
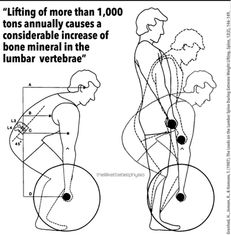
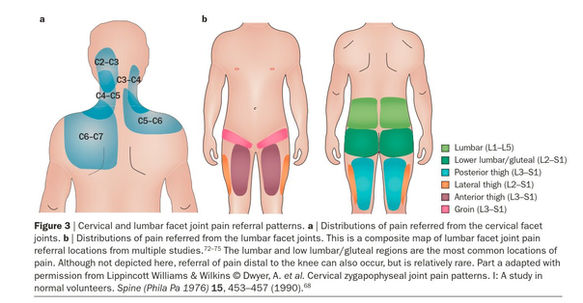
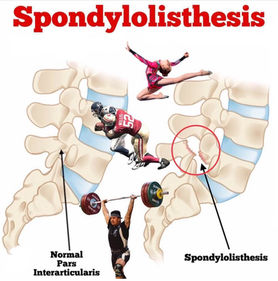
Common medical diagnostic labels for LBP include: Disc degeneration, bulges, prolapses, facet arthropathy, annular tears, spondylosis, spondylolisthesis, stenosis, sacroiliac joint pain.
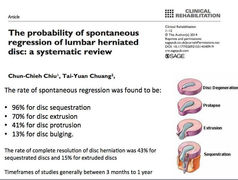
In specific LBP (i.e. presence of pathology), a small group of patients (5%) who present with LBP from slipped disc with associated radicular leg pain with or without neurological deficit, the natural healing history is good. Prospective studies (i.e. research that tracks people over a period of time) showed high recovery rates (over 80%) and reduction of slipped disc at 12 months follow up. Only in some cases where there is progressive worsening neurology and cauda equina symptoms is surgical opinion warranted.
As for acute radiculopathy where pain levels are distressing, pain management and patient reassurance on the natural healing history is important. As pain settles (usually 3-6months), a graduated rehabilitation program needs to be given to normalize movement and return patient back to daily living activities. In the case of stenosis (e.g. lateral recess and central canal stenosis) where pain is disabling, decompression surgery may be indicated should conservative rehabilitation (exercises targeting spine & hip flexibility, extension spinal load reduction and lifestyle factors (obesity and sedentary) has failed. lumbar spondylolisthesis grade (1 to 2) can be managed well conservatively.
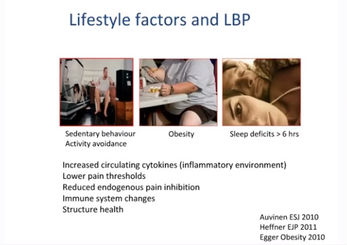
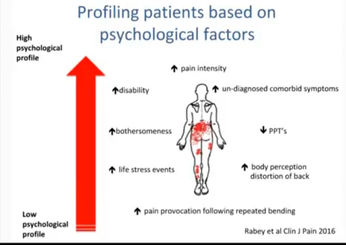
Its really important to also know that one's pain experience is not just about the back. Evidence has also shown factors such as poor sleep habits, high stress levels sustained over time, low mood and anxiety are strong predictors of LBP. This highlights the role that lifestyle, negative affections and emotions factors play to sensitize spinal structures via one's body nervous pain system. This maybe clinically evidenced from a patient presenting with LBP, reporting high levels of low back pain, distress and muscle spasms without or little mechanical trigger - a history trauma, overuse, overload (e.g. sports).
Negative LBP beliefs have also been shown to predict chronicity - ongoing pain intensity, disability levels and work absenteeism14 such as having a negative future outlook (e.g. ‘I know it will just get worse’) and believing that ‘hurt equals harm’ and that ‘movements that hurt should be avoided’ because of fear of pain and/or harm.
In the absence of trauma, pain behaviors such as protective muscle guarding, limping, fear, distress and grimacing, can reflect pain catastrophic thinking (e.g. ‘my back is damaged and I am never going to get better’ and ‘I am going to end up in a wheel chair). Such unhelpful pain behaviors can result in unhelpful straining of sensitive spinal structures, causing pain to persist. These behaviors lead to poor coping strategies (i.e. avoidance and excessive rest), leaving the person feeling disabled and helpless.
Physiotherapists are key healthcare providers for conservative LBP care, being tasked to prevent persistent pain and disability, and facilitating a pathway to wellness and functional restoration.
BACK PAIN GALLERY

FREQUENTLY ASKED QUESTIONS
REFERENCES
-
Low back pain and sciatica in over 16s: assessment and management, National Institute for Health and Care Excellence, Nov 2016, https://www.nice.org.uk/guidance/ng59. [PubMed]
-
Maher C, Underwood M, Buchbinder R, Non-specific low back pain, Lancet 2017 Feb 18;389(10070):736-747. doi: 10.1016/S0140-6736(16)30970-9. [PubMed]
-
Hartvigsen J, Hancock M, Kongsted A, et al., What low back pain is and why we need to pay attention. Lancet 2018 Jun 9;391(10137):2356-2367. [PubMed]
-
Lin I, Waller R, Wiles L, et al., What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high quality clinical practice guidelines: systematic review, BJSM, 2019, Mar 2: doi: 10.1136/bjsports-2018-099878. [PubMed]
-
Saragiotto BT, Machado GC, Ferreira ML, Pinheiro MB, Abdel Shaheed C, Maher CG. Paracetamol for low back pain. Cochrane Database Syst Rev. 2016 Jun 7(6):CD012230. PMID: 27271789. doi: 10.1002/14651858.CD012230. [PubMed]
-
Machado GC, Maher CG, Ferreira PH, Day RO, Pinheiro MB, Ferreira ML. Non-steroidal anti-inflammatory drugs for spinal pain: a systematic review and meta-analysis. Ann Rheum Dis. 2017 Jul;76(7):1269-78. PMID: 28153830. doi: 10.1136/annrheumdis-2016-210597. [PubMed]
-
Qaseem A, Wilt TJ, McLean RM, Forciea MA, Clinical Guidelines Committee of the American College of P. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017 Apr 4;166(7):514-30. PMID: 28192789. doi: 10.7326/M16-2367. [PubMed]
-
Low back pain and sciatica in over 16s: assessment and management, National Institute for Health and Care Excellence, Nov 2016, https://www.nice.org.uk/guidance/ng59. [PubMed]
-
Maher C, Underwood M, Buchbinder R, Non-specific low back pain, Lancet 2017 Feb 18;389(10070):736-747. doi: 10.1016/S0140-6736(16)30970-9. [PubMed]
-
Hartvigsen J, Hancock M, Kongsted A, et al., What low back pain is and why we need to pay attention. Lancet 2018 Jun 9;391(10137):2356-2367. [PubMed]
-
Lin I, Waller R, Wiles L, et al., What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high quality clinical practice guidelines: systematic review, BJSM, 2019, Mar 2: doi: 10.1136/bjsports-2018-099878. [PubMed]
-
Saragiotto BT, Machado GC, Ferreira ML, Pinheiro MB, Abdel Shaheed C, Maher CG. Paracetamol for low back pain. Cochrane Database Syst Rev. 2016 Jun 7(6):CD012230. PMID: 27271789. doi: 10.1002/14651858.CD012230. [PubMed]
-
Machado GC, Maher CG, Ferreira PH, Day RO, Pinheiro MB, Ferreira ML. Non-steroidal anti-inflammatory drugs for spinal pain: a systematic review and meta-analysis. Ann Rheum Dis. 2017 Jul;76(7):1269-78. PMID: 28153830. doi: 10.1136/annrheumdis-2016-210597. [PubMed]
-
Qaseem A, Wilt TJ, McLean RM, Forciea MA, Clinical Guidelines Committee of the American College of P. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017 Apr 4;166(7):514-30. PMID: 28192789. doi: 10.7326/M16-2367. [PubMed]
-
el Barzouhi A, Vleggeert-Lankamp CL, Lycklama à Nijeholt GJ, et al. Magnetic resonance imaging in follow-up assessment of sciatica. N Engl J Med 2013; 368: 999-1007.
-
O’Sullivan PB, Twomey LT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine 1997; 22: 2959-2967.
-
Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull 2007; 133: 581-624.
-
Main CJ, Foster N, Buchbinder R. How important are back pain beliefs and expectations for satisfactory recovery from back pain? Best Pract Res Clin Rheumatol 2010; 24: 205-217.
-
Sullivan MJ, Thorn B, Haythornthwaite JA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain 2001; 17: 52-64.

Available Soon
Additional resource will be available soon

Available Soon
Additional resource will be available soon

Available Soon
Additional resource will be available soon